In part 3 of our series on coaching for health challenges, Alison Carter and Penny Newman explore how health coaching is delivering cost savings and improving organisational culture, and offer practical tips for coaches
If it hasn’t already, health coaching may be coming to the NHS near you. You might not know it, but the person sitting next to you in a GP’s or clinic’s waiting room may already be engaging in coaching conversations about their own health and becoming more motivated and confident to change.
As with other coaching applications, health coaching can be delivered in different ways. Stand-alone services targeted at specific patient groups or conditions and delivered by specialist coaches are the best known method of delivery in the US. What’s newer in the NHS is a health coaching skill-set which can be used by all clinicians as part of a patient’s usual care. The aim of health coaching in this context is to change the conversations between clinicians and patients, to enable patients to self-manage and change behaviour and so improve their own health outcomes.
With greater incentive to change lifestyle habits, take medication correctly and act with confidence rather than calling a doctor when required, patients don’t need as many appointments so it’s an efficient as well as effective approach.
For many clinicians (doctors, nurses or therapists), this requires a change in their own mindset and practice as consultations become a meeting of equals, and less expert driven, drawing on the patient’s own resources, choices and ideas to meet a goal important to them.
The NHS is huge and dispersed. Any change in practice is a big challenge. We know from the literature that:
- Less than 30% (estimated) of sustained change in organisations is successful1
- Leadership at all levels is key to success2
- Large changes in NHS-like organisations need a vision that’s better than the status quo3
- High organisation support is vital to the spread and effectiveness of health coaching4
Case study
Health Education England East (HEEE) took a systemic approach to diffusing health coaching to meet the challenge of improving people’s health behaviours and giving clinicians new mindsets and tools to have a more enabling conversation.
The HEEE health coaching intervention kicked off with a two-day health coaching programme to develop coaching skills for use in part of daily clinical practice. Co-designed and previously piloted by Drs Penny Newman and Andrew McDowell, the programme was delivered to almost 800 clinicians from 46 different NHS organisations during 2013-15. A further eight-day programme was provided for 25 of the clinicians to become in-house clinician-trainers in health coaching for skills transfer and sustainability.
An initial evaluation by the Institute for Employment Studies (IES) indicated high usage of the approach, cost savings, reduction in clinical time and a positive impact on organisational culture. By mid-2016, the programme had been adopted as part of the NHS Innovation Accelerator Programme and more than 3,000 clinicians trained across the country accompanied by a wave of local training success stories in early adopter organisations.
Training based on this approach has now been commissioned in at least five other English regions reaching millions of patients.5 A Health Coaching implementation toolkit was launched in September 2016 to help spread the message about the health coaching to other parts of the NHS and beyond. It can be downloaded for free here:
( www.betterconversation.co.uk)
Health coaching across the East of England wasn’t introduced as a formal top-down policy: sometimes the impetus to use coaching locally came bottom-up from groups of clinicians, or particular coaching champions.
Getting training into place and then working for the patients was not always a straightforward exercise either. There were many barriers to be overcome locally. This may sound familiar to readers who have been involved in establishing a body of internal coaches to deliver coaching to employees or customers or those introducing managerial coaching.
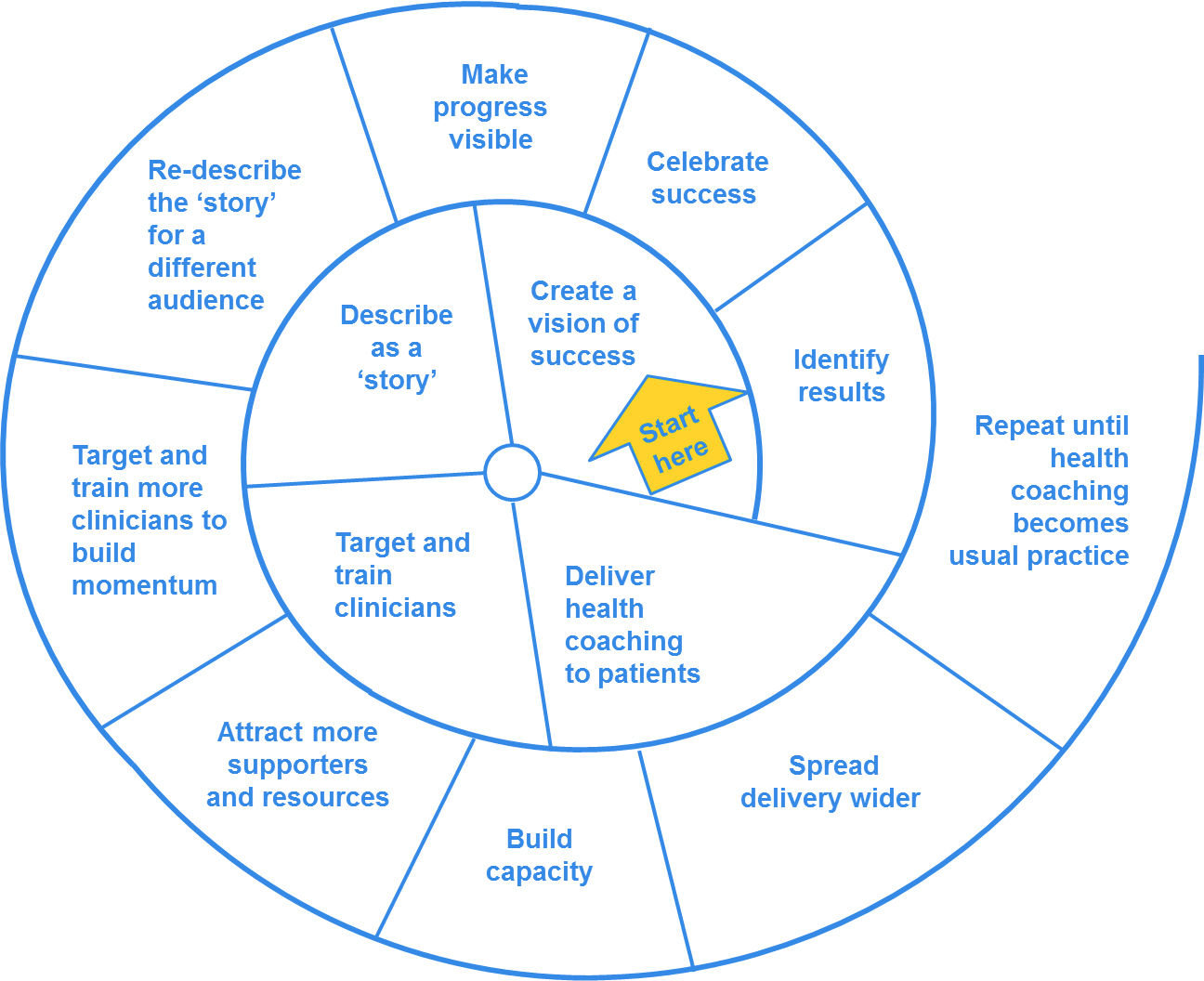
We decided to reflect, document and share the process of spreading and embedding the health coaching message to help others reflect on progress with their own coaching applications. We produced a model adapted from an evidence-based model of large-scale change developed by Helen Bevan and colleagues and used widely by change leadership teams across the NHS. The accompanying commentary is based on discussions with in-house clinician-trainers from eight early adopter organisations across the East of England in February 2016.
The resulting ‘seashell’ model is reproduced in Figure 1.
There are eight prompts to consider when embedding health coaching in services:
- Create a vision of success
Large-scale change begins by identifying a need for change: why it won’t work to carry on in the same old way. Have a clear and understandable vision for stakeholders interested in adopting a health coaching approach, and be flexible on specifics. Link to values and national strategies.
- Describe health coaching
Use a patient or clinician ‘story’ to connect emotionally with people. Talk to the CEO, executive team and clinical leads about health coaching. Be clear about organisational gains, what success looks like and how it is judged. Build evaluation in from the start. Create urgency. Recognise that people are different and tailor the message to the audience. State clearly the support, resources, access or actions needed for health coaching.
- Target and train clinicians
Find a way to convince professionals to take part, if appropriate, or to provide their support. Involve the most influential clinicians locally. Decide where to start: target one service/ward/team and one patient group or have a clear rationale for casting the net wider. Get the training/education team involved to organise and provide venues. Train targeted personnel quickly. If possible, train intact teams as they will support each other in using their new skills with patients.
- Deliver health coaching to patients
The greatest impact will accrue with a critical mass of trained clinicians and targeted service/ward/team to create a common language and culture and so any team member can then follow through with patients. Help clinicians overcome perceived barriers to health coaching in their daily roles if skills are not being used as part of a specific targeted service. Local champions, line managers or mentors can all be tasked to offer support.
- Review
The appearance of success matters, so use collected evidence. Spread the word about health coaching achievements. Connect to national/local strategies. Share new clinician and patient stories to keep health coaching in everyone’s mind.
But be reflective: look for problems. Where is the health coaching not working? What’s getting in the way? What could be done differently? What help is needed?
- Re-describe the ‘story’ for different audiences
If more support is needed, perhaps from funders, cast the net wider. Build on what has already been accomplished. Present at their meetings: use clinical examples of achievements and give a demonstration. If one particular story isn’t engaging, use another description for what health coaching can do.
- Target and train more people
Keep up the momentum. Use resources to support those already trained or to train more clinicians. Target other areas that may benefit.
- Attract more supporters and resources
Continually attracting new supporters is key to spreading health coaching, shifting mindsets and changing practice. Without them, health coaching may well fizzle out or only the few champions who have ‘got it’ will keep using coaching with their own patients. Convince previously neutral people to help.
- Build capacity
If you are pursuing a whole organisation model of health coaching, build capacity and capability to make health coaching sustainable. Get health coaching integrated into management systems. Ask team leaders to put training into individual development plans. Ask HR to timetable introductory slots on induction days. Ask the training/education team to get health coaching integrated into relevant professional requirements.
- Spread delivery wider
Keep going until health coaching becomes embedded in teams, services and across local health systems! For health coaching to become an established and valued tool keep repeating this pattern of re-describing, attracting new supporters and integrating health coaching into corporate systems.
- This article is adapted from chapter 6 of Better Conversation: a Guide to Health Coaching http://bit.ly/2r6q275
- See also: Coaching at Work Health Coaching toolkit (Stephen Palmer):
- Part 1: Key theories http://bit.ly/2rXMfFv
- Part 2: Motivational interviewing http://bit.ly/2rdnZlF
- Part 3: Cognitive behavioural approach http://bit.ly/2rXMkch
- Part 4: Cognitive thinking skills http://bit.ly/2sOX9h6
- Part 5: Multimodal http://bit.ly/2sfnOq7
- Dr Alison Carter is principal research fellow at Institute for Employment Studies and supporter of the Health Coaching Coalition
Alison.carter@employment-studies.co.uk
Penny Newman is a GP and medical director at Norfolk Community Health and Care NHS Trust. She pioneered the development of health coaching in the NHS and is now an NHS Innovation Accelerator Fellow scaling this approach. Penny.newman1@nhs.net
- The article flagged up in the Coaching at Work May/June issue about working with clients around mental health issues will appear in the September/October magazine
- Next issue: How to work with clients around mental health
What clinicians and health coaches say
“ You need management buy-in to spread health coaching. We highlighted our work on health coaching to our chief executive in the context of his vision for self-management and patient empowerment. This led to a big push within the organisation to build on health coaching. The key was to align with national and local agendas and keep linking back to these”
“Our own personal experience of health coaching, the experiences of our patients and the feedback from the clinicians we have trained has been the most useful evidence of success over our first year of rolling out health coaching. We are now working with our organisation to provide more concrete outcome data”
Top tips from health coaches
- Top-level support definitely oils the machinery and counters line manager resistance.
- Don’t introduce health coaching during a time of perceived negatives (eg, after redundancies have been announced). Few people want to, or can, concentrate
on a ‘Bright New Tomorrow’ when today involves uncertainty and potentially insecurity. - Be sure to measure, in cold, hard terms, the effects of health coaching. Anecdotal evidence – the ‘I-feel-better’ accounts – are persuasive in the early days, but at some point executives will demand evidence to ensure monies on health coaching training is being well spent.
- As a by-product of the coaching process, clinicians themselves report having a much better, less stressed and more fulfilling work experience. This doesn’t show up on a balance sheet or a budgetary report, but can make your organisation feel like a better place to work.
FACT FILE AND FURTHER INFO
1 J Bennett and M W Bush, Coaching for Change, New York: Routledge, 2014
2 H H Jorgensen, O Bruehl and N Franke, Making Change Work…While the Work Keeps Changing, New York: IBM, 2013
3 H Bevan, P Plsek and L Winstanley, Leading Large Scale Change: A Practical Guide, Coventry: NHS Institute for Innovation and Improvement, 2011
4 A Carter, P Tamkin, S Wilson and L Miller, The Case for Health Coaching, Cambridge: Institute for Employment Studies/Health Education East of England, 2015
5 P Newman and A McDowell, ‘Life changing conversations: Clinicians’ experience of health coaching in the east of England’, 3-2-147, in Future Hospital Journal, 1 June, 2016, 3(2), pp147-151
6 Reproduced by kind permission of Health Education England East:see www.betterconversation.co.uk for more information